
Innovations from around the UK
The examples below highlight how different areas in the UK have implemented the new NMC Standards.
You can click the individual sections to expand for more information.
England
Background:
The NHS Long Term Plan (2019) explained the need to increase the number of learners in placements across the NHS. To meet these aims, employers need to scale up the ability to offer high-quality learning environments that support workforce development. With regards to the NMC Standards for Student Supervision and Assessment (2018) it has become apparent that we need to change the unsustainable practice of 1:1 mentoring of students and increase placement capacity. In October 2019, Dorset County Hospital NHS Foundation Trust implemented a Collaborative Learning in Practice (CLiP) style model on Purbeck, an orthopaedic trauma ward in response to this. This has been developed as part of a quality improvement project with Trust Board support.
Originating in Amsterdam, CLiP is a model of learning using coaching principles to support students in practice and focuses on the student being an active participant in their learning during their practice placement. This was adopted and piloted in East Anglia prior to being adapted and rolled out in hospital trusts across the country; anecdotally it has proven to be popular with students and placement areas.
Overall project objectives include:
1. To meet the goals of the NHS Long Term Plan (2019) by increasing our placement capacity for learners.
2. To offer a high quality placement experience.
3. To measure the impact of CLiP on the patient experience through a formal audit.
Methodology:
Dorset County Hospital appointed two CLiP Facilitators to ensure practice placement areas had ongoing, hands on support in implementing an enhanced placement experience.
Preparation for the commencement of the student-led zone, the area we are designating to the students, involved ongoing engagement with Purbeck Ward. The ward was initially chosen due to the positive attitude of the Ward Sister and her team. The added benefit was the consistently excellent student feedback, which gave a baseline standard to enable comparison of feedback from the project.
• Increased capacity for students by 100% by utilising a coaching model.
• An allocated student-led zone is run by 3 students on a shift each day supervised by one RN who has had updated training on NMC (2018) Standards for Supervision and Assessment.
• Ideally the students are of varying experience and are able to support and complement each other’s learning.
• Students were encouraged to complete daily learning logs to present to their Practice Assessor at the time of their assessment.
• To develop student leadership skills with the most senior learner coordinating the student-led zone.
• The CLiP Facilitator overseeing this ward made multiple daily visits to ensure ongoing support for all involved with the project.
• Ongoing evaluation will take place. Students, Practice Supervisors and Assessors and patients will be given the opportunity to provide feedback on their experiences.
Learning and future work:
As a formal project our aim is to collect measurement and benefit data including patient, staff and student feedback, safety data and monitoring the actual increase in capacity of learners.
A formal audit of patient questionnaires has been undertaken with support of the Patient Advice and Liaison Service in order to measure the impact of the project on the experience of our patients. The initial patient feedback has shown 100% of patients questioned felt that staff had more time to provide personal care in the student-led zone compared to previous hospital stays and 100% of patients felt that the standard of care they received met their expectations. The ‘Friends and Family Test’ is also being utilised as a method of capturing feedback regarding any student nurses they have engaged with.
In January 2020, our CLiP style practice placement model will be rolled out across two further wards, with a view to increasing to a total of six by September 2020. The pace of the roll out will ensure that our Practice Assessors and Supervisors are well supported in practice, enabling a project that will be sustainable and embedded into Dorset County Hospital culture. In addition, we are aiming to introduce other learners into the project, including Trainee Nursing Associates and newly recruited Overseas Nurses therefore reflecting the evolving needs of the service.

Background:
East Suffolk and North Essex foundation Trust have developed a model of planned associated learning; building on the concept of Hub & Spoke placement allocation, to both improve the learning experience for students as well as increasing the placement capacity.
Developing planned associated learning through Hub & Spoke provides greater access to specialists, resources and opportunities, which can enable the students to gain a greater depth and breadth of knowledge, skill and experience. Providing a greater planned diversity of leaning opportunities provides parity to all students and supports attainment of clinical procedures identified in Future Nurse Standards (2018a).
Overall project objectives include:
1. To enhance the students practice learning experience and opportunities
2. Increase access to and participation in clinical procedures required in the Future nurse standards
3. Increase placement capacity
Methodology:
Utilising a Hub & Spoke model enabled us to increase capacity, by linking underutilised small specialist (spoke) areas to wards traditionally used for long student placements (hub). By planning for each student allocated to the hub ward to spend time in the spoke area, we were able to increase the capacity without having too many learners in the hub area at the same time.
The Practice Education Facilitator (PEF) team worked with the clinical teams to plan hub and spoke areas, which follow the patient journey as well as developing more planned learning opportunities. It was important that we considered placements as not only within a physical space, but as associated guided learning.
Hub & Spoke allows registered practitioners to work together more closely with shared responsibility and interest in student learning to improve skills and knowledge, the quality of our practice delivery and learning achieved. Considering the new NMC Standards for Supervision and Assessment (NMC 2018), our Practice Assessors can be based in a Hub or a Spoke environment, whilst all areas will have professionals acting in Practice Supervisor roles.
A spoke can be identified as an associated environment or a focused theme:
An associated environment
Infographic 1 shows an example of being in different places with different professionals within patient journey.
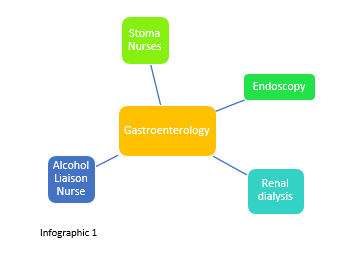
These are determined by staff who understand how the student journey can mirror the patient journey, with the support of the PEF team to co-ordinate initial communication, planning and development of resources.
A focused theme
Infographic 2 shows an example of being in the same or other places with a defined theme to focus on for ‘spoke’ week.
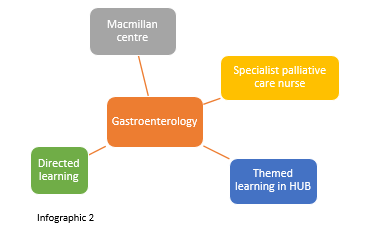
To support the facilitation of student learning, particularly in themed spokes. The PEF team have developed a suite of education resources, with input of relevant specialists e.g. workbooks and the provision of electronic tablets with educational apps.
Learning and future work:
Developing Hub & Spoke ‘planned associated learning’ requires careful planning and co-ordination. Utilising a Hub & Spoke model has resulted in:
• Planned associated learning for all students in hub areas.
• Co-ordinated coaching within defined learning opportunities.
• Increased breadth of understanding of the patient journey within healthcare services.
• Increased depth of empathy towards patients – increased opportunity for developing therapeutic relationships.
• Increased depth and breadth of learning relating to roles and inter-professional working.
• Increased engagement by registrants with consequential improved registrant / student relationships.
• Increased involvement from more specialist areas and specialist practitioners, not only with students but also other practitioners.
• Increased belongingness, person centered care, clinical skills, and professional role development.
• Enhanced the students practice learning experience by shifting the emphasis from a university dictated regime to a more collaborative learning experience where the supervisor and student would be free to shape the students learning experiences.
And of course we are also able to increase placement capacity!
We have started planning the implementation of this model across maternity and are due to commence roll out on our other in-patient and community sites. Currently evaluations are captured as part of the hub allocation through university student evaluations. In our next phase we will capture student evaluation of specific spoke areas and associated learning.

Background:
In 2017 we started to look at how we could both improve the experience of learning in practice as well as increasing placement capacity. Following a review of current models and literature relating to based learning and considering the broader context, especially in anticipation of the NMC Future nurse we began to develop and implement a Collaborative Assessment & Learning Model (CALM), which would meet the needs of our organisation.
This model compliments existing models whilst also further developing the learning culture to embrace the new Standards for Supervision and Assessment (SSSA) (NMC 2018). It moves away from a traditional mentoring role to a more collaborative team approach based on a coaching methodology to supporting learning in practice. Coaching conversations emphasises the need to allow the student to explore and express their understanding, rather than supervisors being directive and telling ‘how to’. Coaching supports the use of effective, specific and timely feedback and signposting and facilitating learning in practice.
In the context of changing student-learning culture, recognition of the reality of the working role and environment of care, is vitally important if we are to support student learning in practice. We think that our new way of supporting practice learning will increase confidence for students and help them gain the ability to think critically, apply knowledge and skills to provide expert, evidence-based, direct nursing care that the NMC states is central to registered nursing practice.
Overall project objectives include:
1. To improve the culture of learning within the organisation
2. To improve confidence and competence of students in practice
3. To promote a quality learning environment
4. To increase placement capacity
Methodology:
CALM has been rolled out in a planned approach over 18 – 24 months. Part of the preparation included several key elements such as:
- Communication with all members of the multi-disciplinary team involved in the delivery of care in the area, i.e. Medical staff and therapists as well as the nurses and non-registrants.
- Standing Operating Procedure for clinical learning environment placement Selection and Monitoring developed
- Training package and associated material developed for delivering coaching conversations
- 1 week student induction, to ensure students suitably prepared to lead care from 1st placement.
- Electronic and hard copy resources developed such as:
- electronic tablet on mobile stand for learners to use in the ward areas
- learning resources related to specific topics
- learning log
- student off duty template
- PEFs facilitate changes and coach the coaches over the first week of implantation then withdraw support as possible
It was important to recognise that whist the underpinning principles would be the same, CALM was not implemented in a “one size fits all” approach. This model provides a framework, which can be adapted to the differing environments, such as critical care, delivery suite or community where a more 1:1 relationship with a patient and student exists.
Within CALM:
- Students will be coached daily be a registered practitioner, utilising expertise of non-registrants as required to meet learning needs
- Students will be allocated patients to lead care for, dependent on their experience, prior learning and learning needs not limited to one bay.
- Students are encouraged to participate in peer learning whilst being coached by a registered practitioner.
- Students will be encouraged to perform new clinical skills based on ability & supervision as per University and Trust guidance.
- Students have access to electronic learning resources at the bedside.
Learning and future work:
As one of our aims was to improve the overall culture of learning within the organisation, we are encouraging this approach to be used for all learners within an area. Although implemented with an initial focus on pre-registration nursing students, we are already seeing areas recognising the benefits of utilising this approach with other learners e.g. our international nursing colleagues who are preparing for UK registration.
Our future work will include more focus on developing inter-professional learning and the inclusion of our allied healthcare students within CALM in a more formalised way.
Background:
Bradford District Care NHS Foundation Trust (BDCFT) have proactively responded to the revised NMC Standards for student Supervision and Assessment (May 2018). They have developed a new framework for student learner support within the organisation to increase capacity and enhance quality within the practice learning environment. The focus for extending capacity is predominantly for first year student nurses, as this is where placement demand is currently the highest.
Overall project objectives include:
1. Stepping Stones extends the NMC Assessment and Supervision roles to include a three-tier placement support framework:
- Practice Assessor (NMC Registrant);
- Principle Practice Supervisor (Registrant on a Professional Register); and
- Practice Supervision Support (Bands 3-5 including newly qualified nurses and Nursing Associates).
2. The programme enables Bands 3-5 (newly qualified and staff who do not possess a recognised teaching and assessing qualification) to develop their skills. It will enable them to effectively support the student learning experience, in a recognised capacity, to become a Practice Supervision Support. This will complement the registrant’s role as Principle Practice Supervisor.
3. By formally recognising and including this large staff group (Bands 3-5) within our infrastructure it will afford BDCFT an opportunity to review an increase in capacity across our nursing services. To meet NMC requirements long-arm supervision of all Practice Supervision Support staff will be provided by the Principle Practice Supervisor who will be a registrant.
4. By completing this programme it will also serve as a pipeline of newly qualified staff who are better prepared for application to a formal Teaching and Assessing qualification (such as SLiP or equivalent).
Methodology:
Staff are invited to express an interest in the programme and to have line manager support. A half day workshop and accompanying workbook cover key areas, including:
- preparing for the arrival of a student;
- how people learn/learning styles/learning theory;
- the role of supervision in the practice learning environment;
- how to develop a lesson plan;
- how to recognise and manage a student who is failing to progress; and
- Practice Assessment Documentation.
On completion of the workshop, staff are assigned to an experienced Principle Practice Supervisor to observe them on a minimum of three occasions supporting the supervision of a pre-registration nursing student. If they have demonstrated and met six mandatory criteria in their knowledge and approach to student support they are then formally recognised in the Practice Supervision Support role and will be added to the Trust student support register.
Learning and future work:
This programme will be piloted in the Trust in September 2019 with a cohort of 40 staff across bands 3-5 (newly qualified). This will be in line with the 2019/20 cohort of first year students due out into their first clinical placements from November. As part of this initial pilot the BDCFT Nursing Development Team would welcome other interested trusts to pilot this programme alongside our local implementation. This would feed into a wider evaluation of its impact in terms of capacity, staff development and quality enhancement of the learning environment and student experience. Moving forwards, this workshop approach will also be considered for use in preparing other professions in supporting Practice Supervisors for the future nurse curriculum.
The photo above show Bradford District Care Trust Nursing Development Team. From left to right: Adele Humphrey (Practice Education Lead), Debbie Cromack (Nursing Development Team manager), Helena Lee (Practice Education Lead).
Background:
This project outlines the approach taken by the West Yorkshire & Humber (WY&H) assessment group, a collaboration of five universities- Bradford, Huddersfield, Hull, Leeds, Leeds Beckett, to the development and implementation of a shared Electronic Practice Assessment Document (ePAD) to support competence assessment of undergraduate pre-registration nursing students across all fields of practice (Learning disabilities, mental Health, Child Nursing, Adult Nursing).
Building upon long standing partnership working across the region’s universities and placement providers, the project illustrates how collaboration and use of an e-portfolio platform, in this case Pebblepad, can facilitate and quality assure practice supervision and assessment, in line with the NMC (2018) new standards for education. With a staged implementation from 2017, upwards of 3,000 students, 15,000 mentors and 200 academics will be using the ePAD when fully operational.
Overall project objectives include:
- A collaborative regional approach, shaped by key stakeholders (students, mentors, educators) from education and practice, to the development and implementation of a shared ePAD to support competence assessment of undergraduate pre-registration nursing students.
- An exploration of pedagogical approaches to promote student and staff engagement with e-portfolio technologies.
- A consistent and staged approach to implementation and support for individuals across the region including resources development to support preparation of students, practitioners and educators in use of ePAD.
- An evaluation of user perspectives of the developed ePAD and selected e-portfolio platform, to support future working.
Methodology:
Strong partnership working across key stakeholders and acknowledgement of user perspectives is a critical element in the development of an ePAD and associated processes to support practice learning and assessment. Integration of ePortfolios across a whole curriculum can support student and staff development in use of technologies and support implementation of an ePAD, and appears to result in positive experiences of ePAD, including perceptions of future relevance and value. Use of an ePAD provides opportunities for students to integrate learning between university and placement settings and promotes timely and efficient communication around student supervision and assessment. Further details of the project design, development and evaluation can be found here.
Learning and future work:
Learning has identified the role that authentic assessment and familiarization with software plays in enhancing student and staff engagement, theory and practice reflection and feedback. Evaluation of user perspectives and engagement with the developed ePAD has identified strengths and areas for future development around:
- Accessibility and Support
- Training and Preparedness
- Communication and Assessment.
Background:
In March 2019 Newcastle upon Tyne Hospitals NHS Foundation Trust trialled a coaching approach to learning on four wards within our organization. This approach was adapted from the Collaborative Learning in Practice (CLiP) model adopted by several trusts in the UK and highlighted in the Shape of Caring review (2014).
Coaching empowers students, allowing them to take responsibility for their learning in a non-traditional environment. The new NMC Standards for Student Supervision and Assessment (2019) state that the student will actively participate in their own learning, “students are empowered to be proactive and to take responsibility for their learning”. The coaching model supports this aspect of the standard as the practice supervisor uses a coaching strategy to allow the learner to identify solutions to practice based problems in a safe environment.
The new standards have moved away from a mentorship approach to a practice supervisor and assessor method. Using a coaching approach replicates these changes, this differs from a traditional 1:1 mentoring role, allowing larger groups of students to work together delivering total patient care under the supervision of a registered nurse which changes daily. The practice assessor (currently sign-off mentor) meets with the students regularly to assess their progress, review feedback and tailor their learning plan to ensure the learning outcomes are attainable and completed in a timely manner.
One of the many benefits of this approach is to combat the escalating concerns from patients that staffing levels are affecting the quality and safety of care delivered. Initial findings from similar projects have demonstrated an improvement in student development which leads to a better prepared and more competent qualified practitioner. We wanted to explore the impact of students working together and directing care.
Overall project objectives include:
- To measure the impact of the introduction of a coaching model on patient safety, particularly in relation to falls, pressure ulcer incidences and rates of infection.
- To pilot a model of practice learning based on coaching which reflects the new NMC standards for student supervision and assessment.
- To increase student placement capacity and monitor the impact of student placement evaluations.
- To explore the educator experience of the introduction of a coaching model.
Methodology:
Within each ward, three to four students, of varying experience, were allocated to care for up eight patients under the supervision of a registered nurse. All care for these patients was planned, prioritised, delegated and delivered by the students with the 'coach' (registered nurse) supporting and guiding the process. The pilot ran for four weeks. Safety data from incident reports for the duration of the pilot was compiled. Post placement evaluations were taken using the standard online placement management system. In addition to this, the coaching lead held weekly sessions with the students to explore issues, reflect and share experiences. A weekly ward visit allowed registrants to discuss any challenges they had experienced.
The Trust recognised the importance of capturing the patient experience as part of the evaluation process of the coaching project, enquiring if the presence of more students on the ward affected the patient experience in terms of privacy, safety and overall experience. A short semi-structured questionnaire was developed and members of the Patient Experience Team visited the pilot wards, once per week over a three week period. The survey was carried out with both patients where students were present in the bays and where they were not, in order that any differences in the experience could be identified. Patients were asked to complete the survey and were given support to do this if required. The purpose of the survey was explained and those taking part were assured that their anonymity would be maintained.
Learning and future work:
Results data is still being collated and analysed, 102 surveys were successfully completed, 72 were from patients where students were present and 30 were from areas without students. Initial findings from patient experience feedback are positive. Patients 'feel' safer using this method as staff are present and visible more often than before. This is possibly due to the practice supervisor being present in the student-led learning bay, supervising and coaching the students. There were a larger number of students on the ward and this may have also impacted on the visibility of ward personnel.
Patients reported that with the introduction of the learning bays (designated areas in which the coaching model of student led care took place) their needs were being met earlier, and students appeared more confident and knowledgeable in this setting. We will be presenting other patient safety data at the 5th Commonwealth Nurses and Midwives Conference 6th and 7th March 2020 and hope to incorporate ongoing data.
In collaboration with Northumbria University we are undergoing further research into the student experience of the coaching model.

Northern Ireland
Background:
At the request of Northern Ireland’s Chief Nursing Officer, Charlotte McArdle, the Northern Ireland Practice and Education Council (NIPEC) is supporting the Department of Health (DoH) in the implementation of the Nursing and Midwifery Council (NMC) Education Standards (2018).
From September 2018 a Northern Ireland (NI) Future Nurse Future Midwife (FNFM) project structure has been established. The FNFM Programme Board have agreed a number of objectives to support the cohesive implementation of the NMC 2018 Education Standards, through a FNFM Working Group and five work streams including:
- Curriculum Development (CD): to ensure the FNFM curricula aligns to the NI Strategic Policy and Transformation Agenda
- Practice Assessment Document (PAD): to co-produce and co-design a Northern Ireland Practice Assessment Document (NI PAD)
- Standards for Student Supervision and Assessment (SSSA): to agree a regional Model for the Standards Student Supervision and Assessment (SSSA) for NMC approved programmes & co-produce a suite of programmes to prepare those taking on the roles identified within the SSSA standards – accessible to all staff
- Practice Learning Environments (PLE): to agree process to ensure quality management of practice placements and explore how current practice learning environments (PLE) can be maximised in the context of the Standards (2018)
- Engagement and Communication: to ensure NI FNFM Project activity is communicated across the region in a timely and accurate way to support implementation.
Co-production and co-design:
In the spirit of co-production and co-design each of the five work streams are Co-chaired by senior colleagues from both practice and education. Work streams membership includes representatives from DoH, Health and Social Care Trusts, Approved Education institution (AEI’s), the Independent Sector, service users and carers, students and other key stakeholders.
A range of FNFM workshops and meetings have taken place to ensure stakeholder engagement and contribution to the development of the various resources and products being prepared to support the outworking’s of implementation of the Standards.
The Programme Board also maintains strong links to the NMC as well as to the other FNFM projects currently running in England, Scotland and Wales to share updates and learning.
Next Steps:
In NI the first cohort of Future Nurse Students are expected to commence on the new curriculum from September 2020. A date for Future Midwife students is to be confirmed. Currently the main focus of the NI FNFM project is preparing evidence to submit as part of the NMC’s Quality Assurance Process for approval.
From October 2019 FNFM information and awareness sessions will be available. These will be co-delivered by representatives from practice and education, geographically spread and open to all staff and students including, but not limited to, HSC Trusts, Primary Care and the Voluntary/Independent Sector.
Work will continue over the coming year to support the implementation of the NMC (2018) FNFM Standards across NI. Partnership working and collaboration with key stakeholders will continue to be a critical part of the process of implementing the new education standards.

Scotland
Background:
A Scottish Future Nurse and Midwife Programme Board has been established to support a ‘Once for Scotland’ approach to the implementation of the new NMC Standards. The chair of the group is Professor Fiona McQueen, Chief Nursing Officer Scottish Government with representation from the NMC, Council of Deans, Scottish Executive Nurse Directors (SEND), National Strategic Group for Practice Learning (NSGPL), Scottish Care, Scottish Collaboration for the Enhancement of Pre-registration Nursing Group (SCEPRN), NHS Education for Scotland, Royal College of Nursing and Royal College of Midwives.
Overall project objectives include:
- To provide strategic oversight, direction and governance to the implementation of the Nursing and Midwifery Council (NMC) Standards of Proficiency for the registered nurse and forthcoming pre-registration Midwifery Standards for Education and Training.
- To consider the future nurse role in its entirety in Scotland.
Methodology:
The Programme Board is supported by six work streams with the following outcomes:
- National model for practice learning support:
- Develop a national model for under graduate and post graduate practice learning with a workforce of practice supervisors, practice assessors and academic assessors, supported by a network of Practice Education Facilitators/Care Home Education Facilitators.
- Develop a national framework for identification, preparation and ongoing professional development of practice supervisors, practice assessors and academic assessors in Scotland with alignment to a refreshed education career and development pathway.
- Quality learning environments:
- Implementation of national Quality Management of the Practice Learning Environment (QMPLE) system for student feedback.
- Implementation of national Quality Management of the Practice Learning Environment (QMPLE) system for student feedback.
- Curriculum context that can be developed through post graduate pathways. Consideration of indicative content for undergraduate topics which will be further developed through post-graduate pathways and associated Continuous Professional Development.
- Refreshed national approaches i.e. national Practice Assessment Document.
- Prescribing-ready content developed (undergraduate) to facilitate commencement of postgraduate prescribing programme V150 following registration.
- A well informed workforce, supported by a national communication plan.
Getting involved and making your views known:
NHD Education for Scotland would like to hear from you. You can make your views, comments or questions known as follows:
- Via Email – N&MPracticeEducation@nes.scot.nhs.uk
- Via Twitter – @NESnmahp or tweet using the hashtags: #Scotfuturenurse #Scotfuturemidwife #yourstandardsyoursay
- Talking to your local PEF, CHEF or University partner

Wales
Background:
The all Wales Pre-Registration Nursing and Midwifery Group is leading on a ‘Once for Wales 2020’ national approach to implementation of new UK Nursing and Midwifery Council (NMC) standards for education (2018). The Group includes representation from service users and carers, NMC Approved Education Institutions, Health Boards/Trusts in Wales, Chief Nursing Office, RCN Wales and other key stakeholders.
The first cohort of students to embark on the new NMC pre-registration nursing proficiencies and post-registration prescribing programmes in Wales will in commence September 2020 subject to successful NMC approval of programmes. Midwifery proficiencies are expected in March 2020 with programme approvals commencing in 2021. There are also imminent standards for Return to Practice, Specialist Community Public Health Nursing and Specialist Practitioner Qualification programmes.
Overall project objectives include:
- A national approach to implementation of NMC Standards for education (2018) in Wales which includes key stakeholder representation and partnerships to co-produce new programme elements, curriculum content, and governance of practice learning and support mechanisms.
- A consistent approach across Wales for nationally agreed elements including:
- A Practice Assessment Document to identify student proficiency in practice.
- Guidance for identification, preparation, allocation and ongoing support of practice supervisor, practice assessor and academic assessor roles.
- An Educational Audit document to review the quality of practice learning environments.
- A student evaluations mechanism for feedback on practice learning experiences.
- A selection and recruitment principles document detailing the values expected of prospective candidates applying for nursing and midwifery programmes.
- An Action Planning Protocol to support students who do not meet required levels of proficiency in practice.
- A smooth transition of new supervision and assessment arrangements across Wales including preparation of the existing workforce to adopt practice supervisor, practice assessor and academic assessor roles in supporting students on pre and post registration nursing and midwifery programmes.
Methodology:
Collaboration and involvement of key representatives continues to be a critical part of the process of implementing the new nursing and midwifery programmes. Local and national discussion forums, partnerships and curriculum planning groups are contributing to the development of future systems, approaches and documentation to support the introduction of programmes across Wales.
Learning and future work:
A series of 34 workshop events hosted by Universities and Health Boards were conducted across all regions of Wales during January, February, March and April 2019. 1034 key stakeholders were represented including service users and carers, students, nurses, midwives, Specialist Community Public Health Nurses, university lecturers and professional leads. Feedback from these forums has also provided detailed information on all Wales elements in the lead up to the first approval events for pre-registration nursing and post-registration prescribing programmes.








